Mediastinum is an anatomical region which is surrounded by thoracic cavity, thoracic entry on the top, diaphragm at the bottom, vertebral column at the posterior, sternum at the front and parietal pleura at the side. Mediastinum is divided into two as superior and inferior with a line extending from the anguli sterni to the fourth inter-vertebral space. The inferior part is named in three parts such as the anterior, visceral and posterior (paravertebral) in proportion to the pericardial sac. Commonly, anterior and superior parts are associated with anterosuperior.
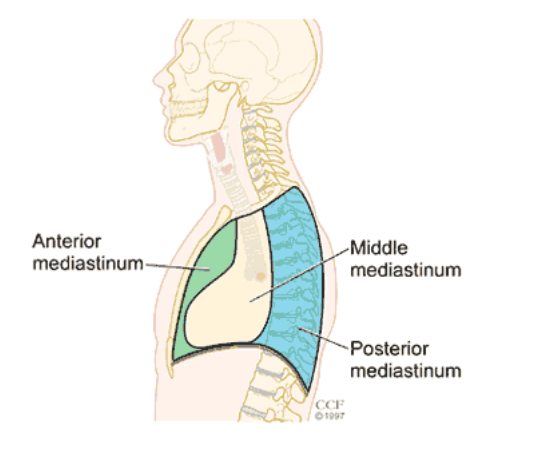
Aortic arch and branches, large venules lymphatics and fat tissue are located in anterosuperior mediastinum. The middle mediastinum includes heart, pericardium, phrenic nerves, trachea bifurcation and main bronchi, both lung hilus and lymph nodes. The posterior mediastinum includes esophagus, vagus nerves, sympathetic chain, descending aorta, azygos and hemiazygos venules, lymph nodes and fatty tissue.
Due to the presence of numerous organs and tissues in different structures in mediastinum; a wide variety of neoplastic masses, cystic lesions and infectious diseases might occur.
While 80% of mediastinal masses stem from secondary masses, the percentage of primary masses are 20%. Primary mediastinal masses can be seen in all ages. However; they are more common in the ages of 20-30 and in males. The incidence has been reported as 4-9/10,000.
Each mediastinal tumor or cyst has an origin in the mediastinum. It has been reported that 54-57% of the lesions are anterior, 9,5-20% of the median and 26-33.4% of the lesions are posterior to the mediastinum. Sabiston and Scott stated that neurogenic tumors are the most common mediastinal mass in the entire age group, and they sort thymoma as second, and lymphoma as the third. For Whooley and his colleagues; the sorting is thymoma, germ cell tumors and lymphoma.
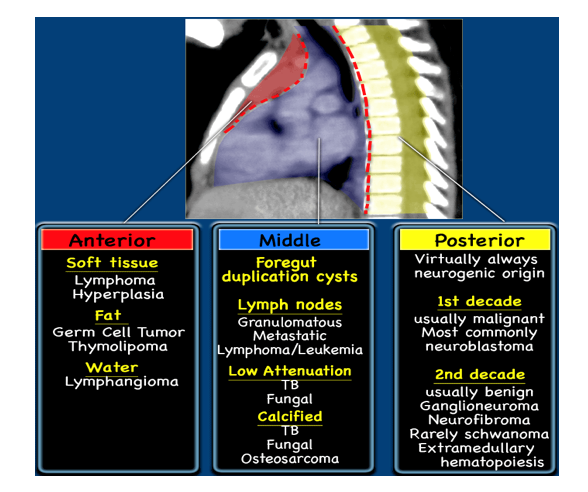
For Duran Yıldız and his colleagues, the sorting is sequential thymic lesions, lymphoma and sarcoidosis. When compared with adults, in children; neurogenic tumors and non-Hodgkin lymphomas are frequent and pericardial cysts and thymomas are scarce. At the same time, the type and the frequency of tumors are closely related to localization. Usually, anterior mediastinal masses are tumors of thymoma, lymphoma, teratoma and germ cells. In middle mediastinum; lymphomas, bronchogenic and pericardial cysts are more frequent. And in posterior mediastinum; neurogenic tumors, bronchogenic and neuroenteric cysts are more frequent.
The division of mediastinal masses according to their places and their frequency are listed below.
Mediastinal masses: Anterior Mediastinum Thymoma – Germ Cell Tumors
- Teratoma
- Seminoma
- Embryonal cell carcinoma
- Choriocarcinoma
- Lymphoma
- Thyroid related lesions -Parathyroid lesions
Medium Mediastinum
- Lymphoma
- Metastatic Masses
- Granulomatous diseases
- Development cysts
- Pericardial cysts
- Bronchogenic cysts
- Vascular Mass and their enlargements
- Diaphragm hernia
Posterior Mediastinum
- Neurogenic Tumors
- Peripheral nerve tumors
- Sympathetic ganglion-derived tumors
- Paraganglionic tissue tumors
- Esophagus lesions
- Diaphragm hernia
What Are the Symptoms of a Mediastinal Tumor?
Almost 40% of people who have mediastinal tumors experience no symptoms. Most of the growths are often discovered on a chest X-ray that is performed for another reason. Symptoms often result from the pressure put by the tumors onto surrounding structures, such as the spinal cord, heart or the pericardium (the heart’s lining), and may include:
- Cough
- Shortness of breath
- Chest pain (somewhat rare)
- Flushing
- Fever
- Chills
- Night sweats
- Coughing up blood
- Hoarseness
- Unexplained weight loss
- Lymphadenopathy (swollen or tender lymph nodes)
- Wheezing
- Stridor (high-pitched and noisy breathing, which could mean a blockage)
- Eye issues (drooping eyelid, small pupil) on one side of the face
Treatment
Surgical intervention is the most effective and the most recommended method for both histologic diagnosis and radical treatment (1,3,14).
For that matter; mediastinoscopy, anterior mediastinomy, transcervical mediastinoscopy, sternotomy, thoracotomy and VATS are the most frequently used surgical methods.
References
- Thomas W. Shields. Overview of Primary Mediastinal Tu- mors and cysts. In Shields TW, LoCicero J, Ponn RB, Rusch VW, ed. General Thoracic Surgery, vol 2, 6th ed. Philadelp- hia: Lippincott Williams and Wilkins; 2005: 2489-93.
- Sabiston DC, Spencer FC: Surgery of the Chest 5th ed. WB Saunders Philadelphia 1990; 498-533.
- Kern JA, Daniel TM, Tribble CG. Thoracoscopic diagnosis and treatment of mediastinal masses. Ann Thorac Surg 1993; 56: 92-6.
- Bradley M, Richardson JD. Primary anterior mediastnila tu- mors in children and adults. Ann Thor Surg 1986; 42: 338-43.
- Capoferri M, Furrer M, Ris HB. Surgical diagnosis and the- rapy in patients with mediastinal space-occupying lesions: A retrospective analysis of 223 intervention with special reference to long-term course. Swiss Surg 1998; 4: 121-8.
- Rubush JL, Gardner IR, Bayd WC, Ehrenhaft JL. Mediasti- nal tumours, review of 186 cases. J thorac Cardiovasc Surg 1973; 65: 216-9.
- Heimburger IL. Primary neoplasms of the mediastinum. ArcSurg 1963; 86: 978-98.
- Davis RD, Oldham NH, Sabiston DC. Primary cysts and neoplasm of the mediastinum: recent changes in clinical pre- sentation, methods of diagnosis, management and results. Ann Thorac Surg 1987; 44: 229-37.
- Cohen AJ, Thompson LN, Edwards FH, Bellamy RF. Pri- mary cysts and tumors of the mediastinum. Ann Thorac Surg 1991; 51: 378-86.
- Brown K, Alberle DR, Batra P, Steckel RS. Current use of imaging in the evulation of primary mediastinal masses. Chest 1990; 98: 466-73.
- Whooley BP, Urshel JD, Antkowiak JD. Primary tumors of the mediastinum. J surg onc 1999; 70: 95-9.
- Yıldız D, Türüt H, Sırmalı H, Altınok T ve ark. öMediastinal kitlelerde cerrahi yaklaşım: 142 olgunun değerlendirilmesi. S.D.U.Tıp Fak. Derg. 2005; 12: 1-5.
- Davids RD, Oldham HN, Sabiston DC. The Mediastinum. In: Sabiston&Spencer Surgery of the Chest, 6th edition. Phila- delphia: WB Saunders Co 1996: 576-611.
- Bacha EA, Chapelier AR, Macchiarini P. Surgery for invasi- ve primary mediastinal tumors. Ann Thorac Surg 1998; 66: 234-9.
- Srivella S, Ford WB, Zikria EA, et al. Foregut cysts of the mediastinum. Result in 20 consecutive surgically treated cases. J Thorac Cardiovasc Surg 1985; 90: 776-82.